While volunteering at the University of New Mexico’s Children’s Hospital in Albuquerque, Quinton Smith quickly realized that he could never be a physician.

Then an undergrad at the university, Smith was too sad seeing sick kids all the time. But, he thought, “maybe I can help them with science.”
Smith had picked his major, chemical engineering, because he saw it as “a cooler way to go premed.” Though he ultimately landed in the lab instead of at the bedside, he has remained passionate about finding ways to cure what ails people.
Today, his lab at the University of California, Irvine uses tools often employed in fabricating tiny electronics to craft miniature, lab-grown organs that mimic their real-life counterparts. “Most of the time, when we study cells, we study them in a petri dish,” Smith says. “But that’s not their native form.” Prodding cells to assemble into these 3-D structures, called organoids, can give researchers a new way to study diseases and test potential treatments.
By combining Silicon Valley tech and stem cell biology, scientists are now “making tissues that look and react and function like human tissues,” Smith says. “And that hasn’t been done before.”
The power of stem cells
Smith’s work began in two dimensions. During his undergraduate studies, he spent two summers in the lab of biomedical engineer Sharon Gerecht, then at Johns Hopkins University. His project aimed to develop a device that could control oxygen and fluid flow inside minuscule chambers on silicon wafers, with the goal of mimicking the environment in which a blood vessel forms. It was there that Smith came to respect human induced pluripotent stem cells.
These stem cells are formed from body cells that are reprogrammed to an early, embryonic stage that can give rise to any cell type. “It just blew my mind that you can take these cells and turn them into anything,” Smith says.
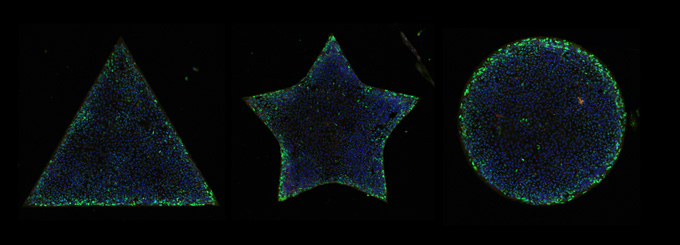
Smith ultimately returned to Gerecht’s lab for his Ph.D., exploring how physical and chemical cues can push these stem cells toward becoming blood vessels. Using a technique called micropatterning — where researchers stamp proteins on glass slides to help cells attach — he spurred cells to organize into the beginnings of artificial blood vessels. Depending on the pattern, the cells formed 2-D stars, circles or triangles, showing how cells come together to form such tubular structures.
While a postdoc at MIT, he transitioned to 3-D, with a focus on liver organoids.
Like branching blood vessels, a network of bile ducts carry bile acid throughout the liver. This fluid helps the body digest and absorb fat. But artificial liver tissue doesn’t always re-create ducts that branch the way they do in the body. Cells growing in the lab “need a little bit of help,” Smith says.
To get around the problems, Smith and his team pour a stiff gel around minuscule acupuncture needles to create channels. After the gel solidifies, the researchers seed stem cells inside and douse the cells in chemical cues to coax them to form ducts. “We can create on-demand bile ducts using an engineering approach,” he says.
color: black;
margin-top: 0px;
background-image: url(“”);
background-size: cover;
padding: 20px;
border: 1px solid #ffcccb;
border-top: 5px solid #e04821;
clear: both;
}
This approach to making liver organoids is possible because Smith speaks the language of biology and the language of engineering, says biomedical engineer Sangeeta Bhatia, a Howard Hughes Medical Institute investigator at MIT and Smith’s postdoc mentor. He can call on his cell biology knowledge and leverage engineering techniques to study how specific cell types are organized to work together in the body.
For example, Smith’s lab now uses 3-D printing to ensure liver tissues grown in the lab, including blood vessels and bile ducts, organize in the right way. Such engineering techniques could help researchers study and pinpoint the root causes behind some liver diseases, such as fatty liver disease, Smith says. Comparing organoids grown from cells from healthy people with those grown from cells from patients with liver disease — including Hispanic people, who are disproportionately affected — may point to a mechanism.
Looking beyond the liver
But Smith isn’t restricting himself to the liver. He and his trainees are branching out to explore other tissues and diseases as well.
One of those pursuits is preeclampsia, a disease that affects pregnant women, and disproportionately African American women. Women with preeclampsia develop dangerously high blood pressure because the placenta is inflamed and constricting the mother’s blood vessels. Smith plans to examine lab-grown placentas to determine how environmental factors such as physical forces and chemical cues from the organ impact attached maternal blood vessels.
“We’re really excited about this work,” Smith says. It’s only recently that scientists have tricked stem cells to enter an earlier stage of development that can form placentas. These lab-grown placentas even produce human chorionic gonadotropin, the hormone responsible for positive pregnancy tests.
Yet another win for the power of stem cells.
Quinton Smith is one of this year’s SN 10: Scientists to Watch, our list of 10 early and mid-career scientists who are making extraordinary contributions to their field. We’ll be rolling out the full list throughout 2023.
Want to nominate someone for the SN 10? Send their name, affiliation and a few sentences about them and their work to [email protected].